“Almost everything will work again if you unplug it for a few minutes… including you.”
~ Writer Anne Lamott.
Despite our sophisticated understanding of various psychological mechanisms that lead to stress, anxiety, and depression in our clients, we have a tendency to conflate the signal for the fire. The alarm bells tell us that something’s burning. Unless it’s a false alarm, the sirens aren’t the problem.
The experience of burnout is symptomatic of a compounded problem. What we need to gain clarity of is what cumulated to the emotional exhaustion.
In his writing about burnout in the medical profession, Richard Gunderman, MD, Ph.D. points out that
“Burnout at its deepest level… is the sum total of hundreds and thousands of tiny betrayals of purpose, each one so minute that it hardly attracts notice. When a great ship steams across the ocean, even tiny ripples can accumulate over time, precipitating a dramatic shift in course.”
This is not a definitive list, but from my perspective, burnout is often the consequence of one of these nine factors:
1. Overworked
Yes, almost everyone is overworked. You could reason that “I love seeing my clients,” “I get energised seeing my clients back to back,” but seeing 6 to 7 clients in a day with minimal breaks in-between, is a recipe for disaster.
It gets more complicated for some clinicians in agency settings. Holding a garden variety of managerial and leadership roles, attending endless (and mindless) meetings evolve to become the norm in their career progression, taking them further and further away from their original calling to be of help. Many do so because they can affect change on an organisational and systemic level. Meanwhile, the chronological clock doesn’t suddenly become charitable. So what do we do? We work harder. And longer hours… And oh, don’t forget to be fully present with the next 5 clients you’re going to see after lunch. (And then scoot home to play with your kids, have dinner and put them to bed, without losing your temper at them.)
Do not mistake exhaustion for laziness. If you are overworked and spent from performing at your work, something needs to be done. A system needs to be in place to replenish you. Not just once, but routinely. [2]
The Lack of Recovery
A point worth emphasising here is a lack of breaks in your clinical practice. The lack of in-between breaks or breathers can have a profound impact on your focus and wellbeing.
Stress is not the problem. A lack of recovery is.
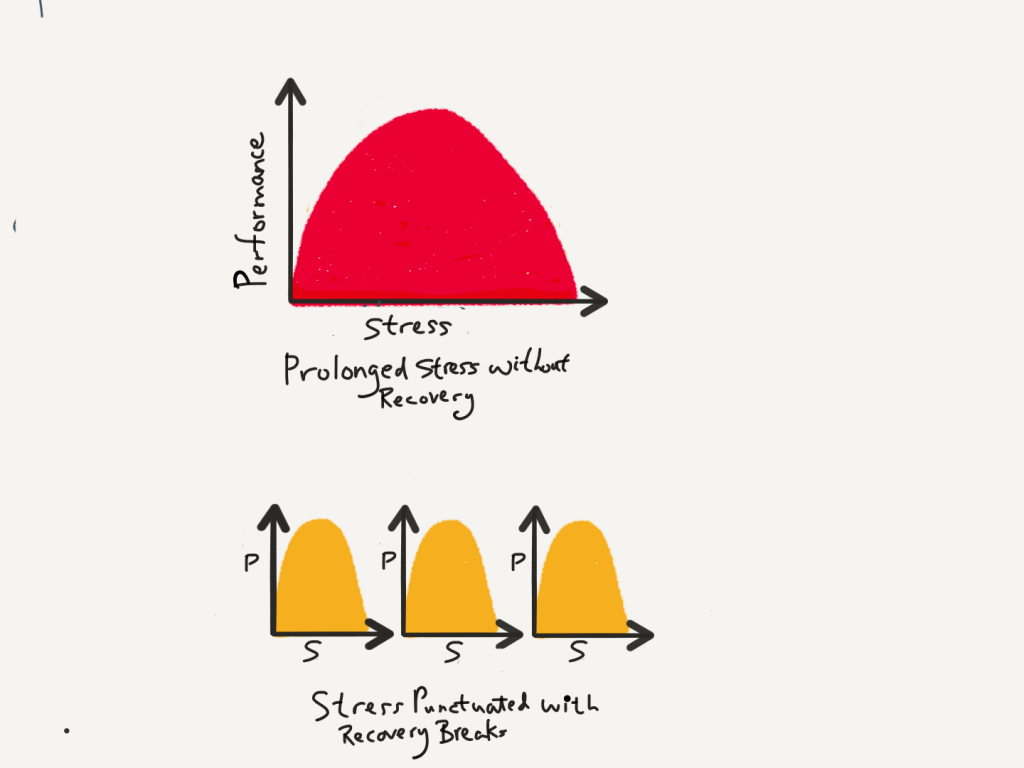
(Adapted from the Power of Full Engagement by Jim Loehr & Tony Schwartz, 2003)
To be open, we need to make the concerted decision—a system of practice (See this talk I gave)—to make room for recovery and being less busy. (I can almost heart the “Buts” amongst my fellow private practitioners. I hear you. But the fact is, let’s think of the long game. We need to not only be sustainable but also, inwardly available. Wearing the badge of honor of busyness is not the most productive thing to endorse, especially being in the helping and healing profession.
2. Toxic Work Environment
John Norcross and James Guy writes, “Psychotherapists are far more comfortable and skilled in changing themselves than in changing the environment. It is as though we are committing in our self-care the same fundamental attribution error we occasionally commit in our professional work. In arriving at causal attributions, we have a tendency to overestimate patient’s dispositions and to underestimate the power of their situations. In other words, we are prone to weigh internal determinants too heavily and external determinants too lightly.”[1]
Context determines behavior. I notice that my colleagues in the mental health profession, are prone to make this attribution error, and fail to acknowledge how a toxic work environment can have a profound impact not just on their performance, but also on their wellbeing.
And the work environment need not be abusive to beat us down. All it takes is for ineffective leadership to neglect creating a nurturing climate that promotes learning instead of an overemphasis on performance. Often, organizations end up measuring stuff that has little value to those whom we serve, which has a trade-off in truly measuring the things of real value. Morale plummets, and no amount of command and control can chastise the team to “shape up.” Instead, climate control is needed, and to refocus and re-energise on creating an environment for deep learning.
3. Ongoing Exposure to Trauma
We work in environments that are in the trenches of losses, traumas, and emotional wounds. The work of being compassionate to another human’s suffering can lead to emphatic distress [3], where wounds of others can open up old wounds of our own. Coupled with being in an unsupportive work environment, this can often feel like we are not being “resilient” enough. Yet, our reality is not just one of “overcoming adversities,” but often it is a dance between our resilience and fragility.
If we travel at the speed of light and not at the speed of life, not only are we overworking ourselves (see point #1), but we will fail to appreciate that the craft of empathy is a slow one.
4. Doubts About Your Effectiveness
The feelings of ineffectiveness is hard to shake off. Its gets more problematic when we conflate “feelings” of ineffectiveness, with actual not doing a good job as a therapist. For example, therapists get surprised when one of the clients does not get better. But, for every 10 clients you see, one of them might deteriorate in your care. [4] On the flip-side, I frequently hear therapists say they have a “stuck” case to discuss, but when we look at the session-by-session trajectories, it turns out that their clients aren’t exactly stuck. It’s us that is stuck with our maps when the terrain looks different that we expected.
When we are not tracking our outcomes, we not only fail to detect who are the ones likely to get worse, in turn, we fail to respond appropriately and provide alternatives.
But if you have been systematically collecting data about your outcomes, and indeed, your outcomes are average compared to benchmarks. Two things can happen. You either 1. Sigh a huge relief and stop there, or 2. Sigh a huge relief and get down to pushing towards your growth edge. The devil is in the details . Seek help to dissect and deconstruct what your clinical data says, and you can begin the wonderful journey of improving your work, inch-by-inch.
And this lack of immediate feedback fuels the unspoken narratives that many therapists have. “Am I any good? What if I am not effective? What if I suck?”
Carl Rogers was right to say that the “data is always friendly,” if we are willing to examine and understand our realities.
Knowing you are effective at your job can be inoculative of burnout [5]. But first, we need to address the next problem in #5. Shooting behind a veil.
5. “Shooting Behind a Veil”
Without using some form of routine outcome monitoring, we are like bowlers prepped with our fancy gear, all poised to roll the magi balls into our lanes—except that the pins are hidden behind a curtain. We are left wandering if we hit a strike or if the ball went into the gutter.
Shooting behind a veil is a sure-fire way to become depressed. The lack of a feed-back loop leaves you to rely on your own clinical assessment. Relying solely on our self-assessment is not only unreliable (see this article I wrote a while back on self-assessment bias) , makes us demoralised, and also makes us prone to making causal inference errors. For example, without a systematic feedback system to inform you on the impact of your work, when a particular session didn’t go well according to our own clinical interpretations (recall: our own perspectives are unreliable), we might think it’s because of us not adhering to a particular model or protocol well enough.
Some therapists say they circumvent self-assessment bias by obtaining client’s verbal feedback. I think that’s critical, but not sufficient. That’s because it isn’t systematic, and neither does this help us to step outside of ourselves and aggregate the data to figure out how effective we are. Renowned business consultant Peter Drucker quipped, “What gets measured, gets managed.”
Numerous studies now point to the practical benefit of integrating outcome measures into clinical practice[6], and more therapists are now beginning to see the benefits for themselves. Seeing the impact of your deliberate practice efforts on client’s outcome over the long haul is remoralising.
6. Overwhelmed and Lack of Directionality in PD
Two of the most common challenges I hear from clinicians all over is that they are overwhelmed and lack a sense of clear directionality, or what to do to make real gains on their road of professional development.
These two factors have an intertwining relationship. In part, we lack a sense of clear direction because we are inundated with some much information to wrestle wit. On the other hand, we are overwhelmed because our intentions are often thwarted before we can see and think clearly about our needs for development.
Note: Keen to develop an individualised professional development plan to raise the bar of your performance? Join Scott Miller and I this August in Chicago for a Deliberate Practice 2-Day Intensive workshop.
7. Isolation
In the practice of therapy, we face a grim possibility of what the poet, Charles Bukowski calls “alone with everybody.”
Ever though I intentionally set out to be in a group practice, I rarely get a chance to interact with my colleagues. I could easily get caught up with busyness—seeing clients, finishing case notes and reports, making phonecalls and replying emails— and not see the light of day, until the sunsets; time to go home. Daddy duties.
In order to break the isolation, I make sure I speak with a close colleague (we call this our mastermind meetings) on a regular basis. David Whyte reckons a good diagnosis of our lives is to look at our friendships. Make sure you connect with folks outside of family and work.
If we are to over-come each of our own plateaus, it is vital we treat the practice of psychotherapy more of a team sport, and less of an individual effort.(See previous article on Scenius vs Genius.
8. Extraneous Events
Things happen in life can happen that is not within our control, like the death of a friend or family, illness, injury, etc.
To expect that therapists are supposed to switch-off and continue to deliver therapeutic service is expect us to behave like bots. While we care for others, care must be taken to attend to the demands of our lives. The practice of psychotherapy requires attention on our own wellbeing, so as to avail ourselves for others whom we serve.
9. Life’s Calling You Into a Different Direction
We don’t talk a lot about this. It is common to speak of folks who make a career switch into the helping profession, but we rarely talk about moving out of this field.
Sometimes, life compels us into a different path. And the skills set obtained in in the practice of psychotherapy is invaluable, and can be transferrable if the knowledge is harnessed. Not attending to these signs can drag you down. I’m not saying to quit your job immediately if this happens, but it certainly is worthy to consider the implications if you do not feel that the practice of therapy is making you come alive.
The Way Out
Once we get pinpointed on the problem at hand, the solution is just around the corner. Here are two key questions to guide your attempts.
1. Be specific when you diagnose burnout. Create a higher definition of the problem. Which ones apply to you? Write it down, and list down the factors that contribute to this problem that led to you feeling burned out.
For example, if you be honest with yourself, is life calling you into a different direction? What are the signs? What are the pull factors?
“Don’t ask yourself what the world needs. Ask yourself what makes you come alive, and go do that, because what the world needs is people who have come alive.”
~ Howard Thurman, The Living Wisdom of Howard Thurman: A Visionary for Our Time
2. Once you have a definition of the problem that led to burnout, create not just a goal, but a process of how to address this, on a systematic and disciplined (but not regimented) basis. We cannot resolve the problem of burnout with a “one-hit” attempt; it needs to be resolved on a regular “drip by drip” basis. Zig Ziglar would say, “People often say that motivation doesn’t last. Well, neither does bathing. That’s why we recommend it daily.”
For example, if you are overworked, overwhelmed, and lack a sense of direction in your professional development efforts, make sure you build in rhythmic periods of rest and recovery. Plus, seek out a consult to help you design an individualised plan.
More: If you are a supervisor who wants to help your supervisees achieve better outcomes through a focus on their development, join us for the 6th batch of the in-depth (and highly personalised) online course, Reigniting Clinical Supervision. Registration closes this Friday, 3rd of May, 2019). More than a hundred practitioners around the world have gone through this course. Not convinced? See what they say.
~~~
In the 1979, Neil Young sings in Hey Hey, My My, “…It’s better to burn out, than to fade away.”
Perhaps this false dichotomy pushes us to the unnecessary brink of demanding more of ourselves, as if that’s the striving of true excellence [Add link on excellence vs perfection]. Like standing on the edge of a cliff, it’s better to seize the opportunity to see clearly on what’s needed to rekindle our original desire of what brought us into the helping profession in the first place. And, more importantly, tend to the wounds of being burned, tenderly.
“Almost everything will work again if you unplug…”
~~~
I love this poem by the late Irish writer, John O’Donohue.
For One Who Is Exhausted, a Blessing
When the rhythm of the heart becomes hectic,
Time takes on the strain until it breaks;
Then all the unattended stress falls in
On the mind like an endless, increasing weight.
The light in the mind becomes dim.
Things you could take in your stride before
Now become laborsome events of will.
Weariness invades your spirit.
Gravity begins falling inside you,
Dragging down every bone.
The tide you never valued has gone out.
And you are marooned on unsure ground.
Something within you has closed down;
And you cannot push yourself back to life.
You have been forced to enter empty time.
The desire that drove you has relinquished.
There is nothing else to do now but rest
And patiently learn to receive the self
You have forsaken in the race of days.
At first your thinking will darken
And sadness take over like listless weather.
The flow of unwept tears will frighten you.
You have traveled too fast over false ground;
Now your soul has come to take you back.
Take refuge in your senses, open up
To all the small miracles you rushed through.
Become inclined to watch the way of rain
When it falls slow and free.
Imitate the habit of twilight,
Taking time to open the well of color
That fostered the brightness of day.
Draw alongside the silence of stone
Until its calmness can claim you.
Be excessively gentle with yourself.
Stay clear of those vexed in spirit.
Learn to linger around someone of ease
Who feels they have all the time in the world.
Gradually, you will return to yourself,
Having learned a new respect for your heart
And the joy that dwells far within slow time.
See also previous article on What Burns You Out?
Footnotes:
[1] Leaving It at the Office: A Guide to Psychotherapist Self-Care, First Edition (p. 153), by John C. Norcross Phd; PhD James D. Guy Jr., 2007. This is a recommended read. I see that there’s now a 2nd edition (and a new co-author) to this book.
[2] The First Kiss: Undoing the Intake Model and Igniting First Sessions in Psychotherapy by Daryl Chow, 2018.
[3] Zen Roshi Joan Halifax notes that a better way to describe compassion fatigue is to call it empathic distress.
[4] Hannan, C., Lambert, M. J., Harmon, C., Nielsen, S. L., Smart, D. W., Shimokawa, K., & Sutton, S. W. (2005). A lab test and algorithms for identifying clients at risk for treatment failure. Journal of Clinical Psychology, 61(2), 155-163. doi:10.1002/jclp.20108
[5] Francoise Mathieu, Mark Hubble & Scott Miller. Burnout Reconsidered in Psychotherapy Networker.
[6] Boswell, J. F., Kraus, D. R., Miller, S. D., & Lambert, M. J. (2013). Implementing routine outcome monitoring in clinical practice: Benefits, challenges, and solutions. Psychotherapy Research, 25(1), 6-19. doi:10.1080/10503307.2013.817696


Great article on burnout Daryl.