Most of the time, we are solving for specifics.
In the natural sciences, however, nature does not solve for specifics, but it solves for patterns. Paraphrasing Agriculturist Wendell Berry (1981), Janine Benus described the process of solving for pattern as
Finding one solution that solves many problems without creating a new one.”
What therapists do on an individual client-by-client level is to be open, responsive, and adaptive to the needs of each person (see Adjustable Seats). However, when it comes to “Solving for Patterns,” instead of trying to figure out how to help a person on a case-by-case-basis, we also need to learn how to extract principles and transfer the learning to other similar situations.
This is more difficult than trying to fix a specific problem, because this requires not only the ability to learn, prevent wrong conclusions, but also the ability to generalise and adapt the learnings into another context. Author of Transfer of Learning, psychologist Robert Haskell says that over the last 9 decades, individuals and academia have failed to achieve tranfer of learning on any significant level. Duped the “Holy Grail” of education. Although transfer of learning is universally recognied as fundamental to all learning, paradoxically the current evidence suggest that it seldom happens in instructional settings.
Returning to Wendell Berry, he points out an important distinction between good and bad solutions
Bad Solutions:
- “A bad solution solves for a single purpose or goal, such as increased production.
- It is typical of such solutions that they achieve stupendous increases in production at exorbitant biological and social costs.”
Good Solutions:
- “A good solution acts within the larger pattern the way a healthy organ acts within the body.”
- “A good solution solves more than one problem, and it does not make new problems.”
- “Good solutions have wide margins, so that the failure of one solution does not imply the impossibility of another.”
In other words, compared to a bad solution, a good solution is actually a shortcut. It’s not only more efficient, but also less taxing in the long run.
Quiz
Meanwhile, let’s take a quick segway.
Solve this pattern:
8, 10, 12, x
What is the number x?
My Solving for Patterns
How does the idea of “Solving for Patterns” apply to my clinical practice? For the sake of comparison, I’d first describe what I learned from my dataset earlier on from the periods of 2004-2009 based on my work in a private hospital (1 year only), plus the subsequent work in a public psychiatric hospital setting in Singapore. When I first examined my outcomes based in Singapore, I was surprised by two patterns:
- As I was systemic thinker, I thought of myself to be apt in working with couples, families, and individuals with relational concerns. However, my outcomes with such issues turned out to be the worst performing group in my data.
- Meanwhile, even though I had been a youth worker for a few years prior to practicing as a psychologist, admittedly, I found working with youths hard work. It took alot more out of me. And what did my dataset say? While their alliance trajectories have a much more “see-saw” than adults, their outcomes out-performed the adult population.
The first discovery about my weakness was sobering, especially since I prided myself to be a family therapist/systemic thinker. The second discovery, was at first, somewhat conflicting. But it soon made sense. I did pour more resources and energy, and I was way more flexible in my approach with youths, so much so that sometimes, the conversations didn’t sound “therapy-like” at all. In fact, I worried that if our governing body heard what I was doing, they would boot me out of the psychology clubhouse.
With the youths, we talked about their friends, the music they were listening to, the movies they watched, the latest social media viral post, etc. In addition, I became less “shocked” whenever I saw the alliance data peak and dip from one session to the next. As I soon picked up, youths seemed to tell me like it is. No holds barred (check the PHRASING) All I did was do my best to learn from their experience by seeking “contrast” questions (e.g. “Help me understand, how come today’s session lower/higher than the previous? What gives?”).
By the way, contrasting their experience from the previous sessions turned out to be a fruitful exercise that I ended up generalising to the general population that I was working with as well. But that meant that I had to be primed to their on-going alliance trajectories.
Back in 2005-06, I was so worried if I was effective at all. (“What If I suck?”). As time progressed, I had to constantly reminded myself that the aim was to measure growth, not competence. This meant stepping away from a competency-based mindset, and more a deep learning perspective. (Listen to this podcast episode to see why my history with “performing” made me re-think about learning. )

About a year and half ago, I relooked at my dataset in an attempt to once again “Solve for Patterns”. Because I no longer worked in a psychiatric setting, I decided to focus my analysis based my current private practice setting in Western Australia, which I’ve been since 2011.
Here’s what I didn’t find:
- No clear difference in outcomes amount differenting presenting issues.
- No clear outcomes difference between private paying client and what we call “Bulk Billers” (when clients are either on a disability pension or are not financially able to affort sessions, I make this exemption for about 10% of my caseload). This surprised me.
- No gender differences in outcome.
- No age group differences in outcome.
In short, all the obvious client factors differences didn’t pop with any signals.
Although somewhat dismayed, I decided to press on and dig alittle further. I began to parse my dataset between those who achieved good outcomes versus those who didn’t. (In case you are wondering, this was done manually on a spreadsheet. No fancy SPSS or other stats program. If you like to see more about this spreadsheet approach, watch Scott MIiller interview with practitioner Michael Harloff https://youtu.be/qAVDrkJFrxE)
My Patterns of Unsuccessful Cases
Here’s what I found in my caseload, (N = 631), comparing between the successful and unsuccessful groups:
1. Trajectory of Outcome Differences:
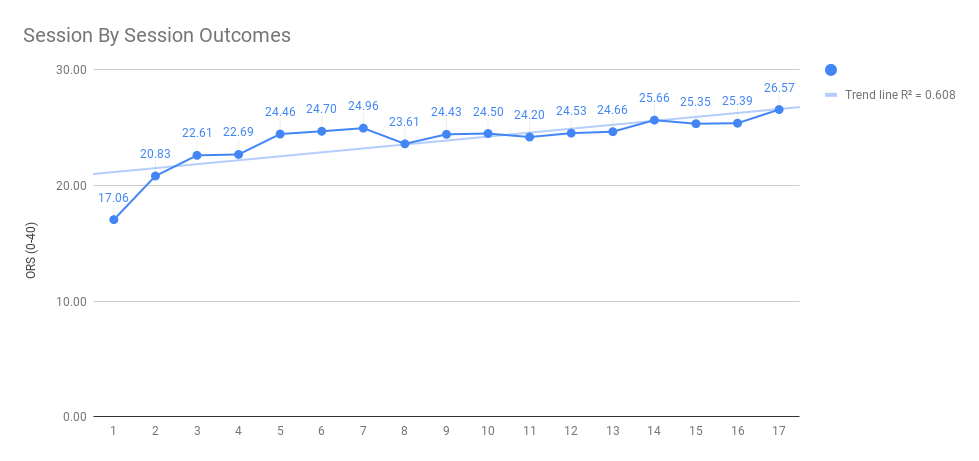
Take a look at the differences in outcomes between the successful and unsuccessful cases
Successful Cases
Unsuccessful Cases
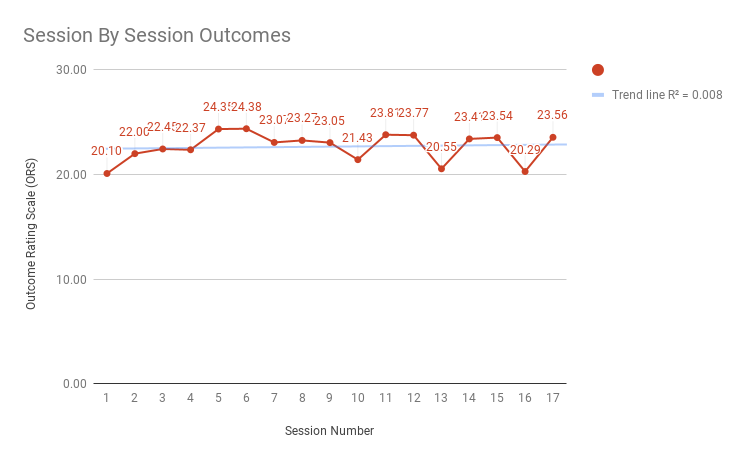
Consistent with research findings, if I were to be successful, on average, change does happen earlier rather than later. This was also consistent with my own outcomes data since 2005.
Implications:
- Clinical Decision Tree:
This affirms my use of a “fast-and-frugal” clinical decision tree, that if a client was not experiencing therapeutic gains by the 4th to 5th session, my first checkpoint is that I’d need to seriously re-evaluate the direction I am taking and discuss this with the client.
My second checkpoint is that if things are still not improving at 6th session, I’d have to seeking consultation with my clinical supervisor.
Finally, if there is still no improvement around the 8th to 10th session, I’d have to consider a couple of other things:
a. Tap into external resources (e.g. group work, community activities)
b. Consideration of medication if relevant and client is open to the idea
c. Consideration of transfer to another colleague (note: This needs to be handled sensitively and with care, as you do not want to seem like you are abandoning a client when things are tough. Typically, I amke htis clear from the get-go that if I’m not going to be effective with them, I would be open to discussion and considering alternatives.)
Remember, a meaningful clinical decision tree is not a rule but a guide that I use to help me have clarify my decision making; not force-fit sqaurepegs in a round hole. Other Supervisors and supervisees in the Reigniting Clinical Supervision course have found this as a useful guide as well. - Placing My Bets
This raises an interesting question: Does this mean that everyone improves earlier rather than later? Of course not.
When a client is not experiencing therapeutic gains between the 4th-8th session, as measured by their outcomes (i.e., not just symptom reduction but global wellbeing), I have to make the collaborative clinical judgement whether to “place my bet” to persist, or to re-think the process. That’s why having the clinical decision tree at the outset is useful. Instead of being reactive, I can be adaptive each step of the way.
For specifically, I know from my outcomes data, that if a client hasn’t experienced meaningful benefits by the 8th session, the odds of that person improving later on is less than 10-20%. What I’m doing is to marry my clinical intuition with the clinical data, so as to make better decisions. This way of thinking tames my optimism and keeps my feet on the ground.
2. Trajectory of Alliance Differences:
Now that we have looked at the trajectory of outcomes, let’s look at the same dataset of clients and examine the differences in alliance between the successful and unsuccessful cases.
Successful Cases
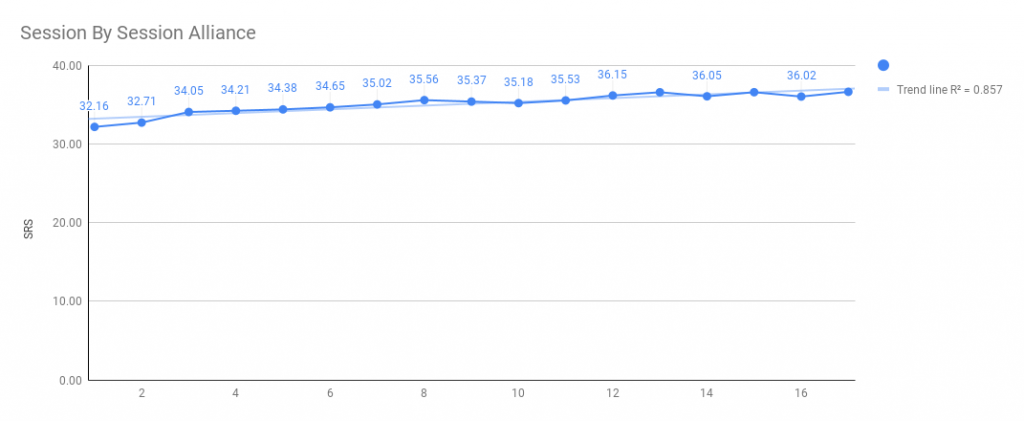
Unsuccessful Cases
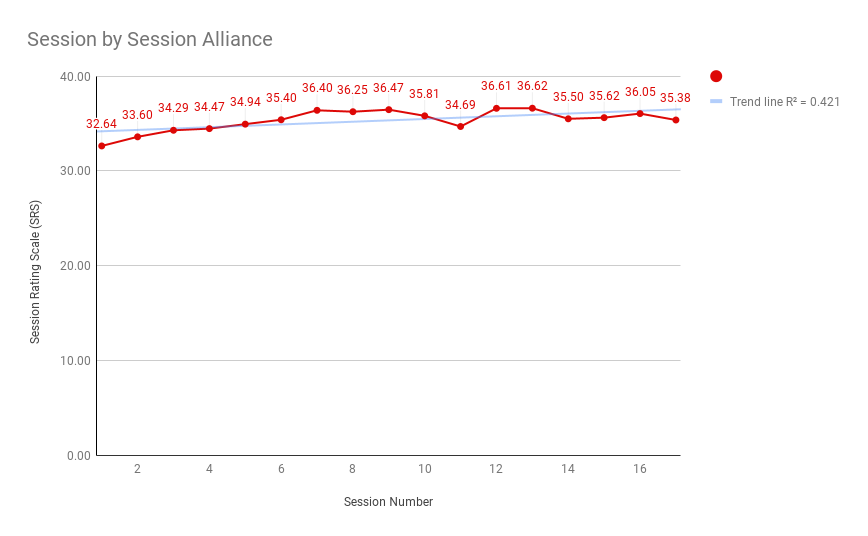
Upon visual inspection comparing both the alliance graphs, there doesn’t seem to be much difference. There seemed to be a slight improvement of engagement over time for both. However, the R-squared differences seems large (successful cases R-squared = 85%; unsuccessful cases R-squared is 42%). Briefly, R-squared is a measure of goodness-of-fit to the linear regression model (i.e., the blue trend line that you see in the graph).
For example, as mentioned in this webpage, the R-squared for the the graph above is 15%, and the one below is 85%. In other words, when the data points are closer to the regression line. the regression model accounts for more of the variance.
In other words, the successful cases in my caseload on average, seemed to have a more gradual improvement overtime, as compared to my unsuccessful cases. Caveat: I’m still not sure about this. I have not done any naunced statistical analysis on this, as one could examine the variability between-clients (i.e., comparing Person A with Person B, Person C, etc) and within-clients (i.e., session-by-session). At such, I don’t have any direct implications based on this level of comparison. Which brings us to the next 3 points.
3. Lack of Consensual Focus
Looking at the numbers alone is not going to yield much. I started to “leave the numbers” and look at the individuals that are represented by the clinical data.
When I looked into the case specifics, several cases in the unsuccessful cohort had lack of goal consensus/directionality/agreed focus.
This was intriguing because this coincided with Bruce Wampold and Zac Imel’s analysis of the psychotherapy outcomes literature. Agreement on the goals of treatment is not studied as much in research, compared to treatment differences, but it has such a high impact on client outcomes!
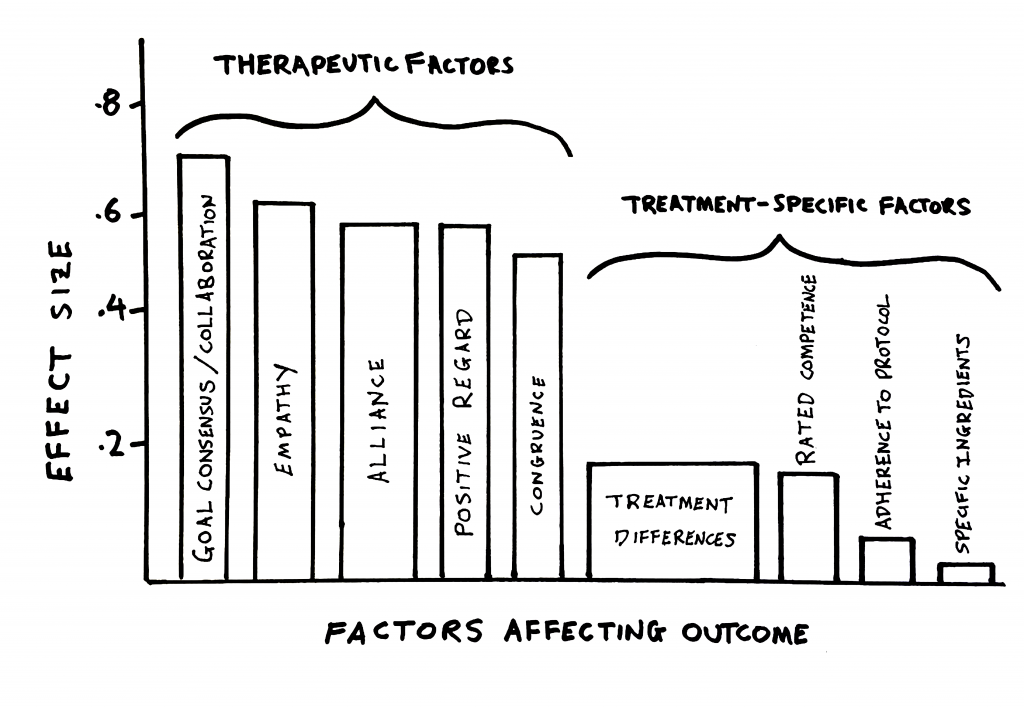
Note: thickness of the bars roughly represent the amount of studies done in those specific areas.
Implications:
This has huge implications for me. I poured my deliberate practice efforts into this area. I returned to my learning project on developed clear directionality and revisited those cases that I have not succeeded in helping.
Take a peak at one of the modules in the Deliberate Practice Web-Based Workshop, where we take a deep dive into an example of my learning project on develop a clear focus.
More recently, I have began to ask client’s to complete an ultra-brief personalised goals survey. Indeed, sometimes the “goal” is to figure out the goal. At other times, I’ve found that my estimation of what’s vital to focus on is worded quiet differently from my clients! This has been a useful conversation piece to have as they elaborate from their point of view with me, and for me to bring into speech on why I thought other areas might be useful to consider too.
For now, the learning project is ongoing. As Singaporeans like to say, there’s “room for improvement.”
4. Lack of Playfulness
As I dug into the cases based on the patterns I’ve found from the clinical data, I’ve also noticed that, from a felt-sense, I was less playful and more rigidifed in several of the poor outcome cases.
This was an important signal for me, as I value a sense of finding a way to speak the unspokens, and create room from both parties to be flexible.
One could also argue that me feeling less flexible might be an effect of the client on me. Either way, it would be safe for me to assume that me feeling constrained is not going to help the other person.
As the researcher and author of Play, Stuart Brown would say, “The lack of play should be treated as serious as malnutrition.”
Implications:
- Stay Playful:
This simple reminder to myself has been useful enough. This doesn’t mean that I act silly, but rather, I allow myself to exercise more creativity… and levity. I also need my body to feel flexible in therapy, so sitting on a chair with wheels promotes that a little more than a chair that’s stationary. - Speaking the Unspokens:
Strangely, one of the side-effect of noticing this pattern was that I found myself challenging my temperament of high agreeableness. When I have a point of view that is different from the client, I continued to learn and invite myself to give voice to the “other voices” at the back of my head. I had to make sure it was not just me speaking disinhibitedly, but rather, in service of the therapeutic intent. For example, I found myself speaking about “junk values” and a lifestyle that was keeping a particular young person being flooded with uncontrollable anxiety attacks.
5. Too Abstract
Finally, I was able to extract this learning point only because I have a formal process of eliciting feedback at the end of each session (i.e., using the Session Rating Scale).
As I looked through my casenotes, I noted that when there was a dip in the alliance, a handful of clients told me similar things: I was too abstract and didn’t provided more concrete strategies and/or direction.
Implication:
- I returned to a therapy learning note # 225 I made on Apr 2018. “Climb up and down the ladder of abstraction.” This means that I have to learn to come down to the ground more often and be more specific. It’s so easy for me to go off with the fairies. I need to help those clients take specific actions based on specific principles, and not leave them with just ideas.
For more on useful feedback to the fullest of advantage, see the following:
How Do You Get Better At Eliciting Feedback?
To Get Useful Feedback, Seek Contrast: Compare Within the Person’s Experience, Not Between Persons.
How Do You Get Better at Receiving Feedback?
Solving for True Patterns
Let’s return to the quiz when had at the beginning:
8, 10, 12, x
What is the number x?
Next. What If I told you that the answer is 15, and that the next 2 numbers are 18 and 21?
8, 10, 12, 15 ,18, 21, x?
Solving for patterns requires that we know when there’s is a true pattern, and when there isn’t.
Give that this post is about analysing your data with your closed cases, in future posts, I will be addressing about what we can do as with our active caseloads from the perspectives of “solving for patterns.” In addition, I hope to also address the topic of whether we should be working on our weaknesses or strengths (or both).
My hope is that you take the time not only to systematically collect your outcomes and use outcome measures to help you be highly adaptive, but also help you solve for patterns, so as to improve your outcomes for more people that you are working with.


6 Responses
[…] In this week’s therapy tip of the week, we are going to talk about the subject that you as a psychotherapist would be more than familiar with–except that it’s not what you expect. ⏳ Time Stamps: 00:00 Introduction 01:08 Three Parts of Working Alliance 01:53 Perspective Taking vs. Perspective Getting 03:14 Highly Effective Therapists and Lower Initial Working Alliance Ratings 03:43 Tip: Compare and Contrast Between Sessions Note: Any personally identifiable information in clinical examples used are changed, in order to protect their confidentiality and privacy. 📕 Resources/ Related Links: 1. http://darylchow.com/frontiers/altered/ 2. http://darylchow.com/frontiers/solvingforpatterns/ […]
[…] my outcomes looking for patterns that might be play out in my client data (see blogpost Solving for Patterns), looking at the differences between successful and unsuccessful cases, 1 out of the five patterns […]
[…] really hit home from me when I was examining my outcomes over the years (see this post, Solving for Patterns). Out of the five patterns, one of them I discovered regarding my poor […]
[…] Active Contemplationi. Solve not just for specifics, but solve for patterns. What can you learn about the people who dropped out from treatment prematurely?ii. What can you […]
[…] I wrote about the value of keeping a playful spirit in my clinical practice in this post, Solving for Patterns.The idea of levity has been more helpful than humour. I don’t have to be comedic or add the […]
[…] Once she had enough cases for a reliable, evidence-based analysis of her clinical performance, she began the process of identifying the outcome goal. In an effort to identify the area with the most leverage on improving her results, she created a spreadsheet listing each client’s data (i.e., outcome and relationship scores) and other details. In a separate column, a distinction was drawn between those she treated successfully (reliable improvement) an unsuccessfully (lack of reliable change, deteriorated, or dropped out after the first session). Next, with the spreadsheet open on her computer, she starting reviewing the progrsss notes of her closed cases, sorting and “solving for patterns.” […]